Leg ulcers are skin lesions arising from bad blood circulation into the veins and/or the arteries. They affect 1 in 100 1 people, mainly women, and up to 3% of the over 65s 2. These ulcers can take a long time to heal and need to be taken seriously as soon as they appear in order to prevent them from worsening.
What is a leg ulcer ?
Located on the lower third of the leg (under the knee), leg ulcers are chronic wounds that have not healed after 6 weeks. The wounds may be caused by a knock, by scratching, and sometimes can appear on their own.
Leg ulcers take different forms:
- Venous leg ulcers (comprising 70% of cases (3)): related to poor venous circulation. They are superficial in most cases, with inflamed, uneven edges. Venous leg ulcers are painful and usually located around the ankle.
- Arterial leg ulcers (comprising 10% of cases (3)): related to poor arterial circulation. They start out as a small cut with uneven edges on the leg or foot. Gradually becoming deeper, arterial leg ulcers can even go on to reveal the tendons or the bones, as they become progressively necrotic (can turn black). They are generally very painful.
- Mixed leg ulcers: related to poor arterial and venous circulation. Signs of a venous ulcer and an arterial ulcer are present at the same time.
How does a venous ulcer form?
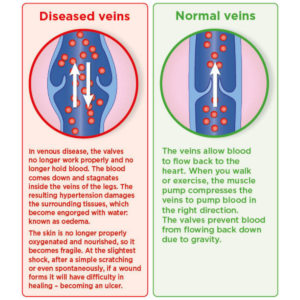
A venous leg ulcer is a sign of chronic venous insufficiency, which prevents the blood flowing normally in the leg veins. Blocked along its usual path, the blood stagnates in the leg veins, and goes on to damage the tissue and break the skin.
This is why treatment should come with an in-depth diagnosis, to identify the cause of the venous failure.
Various factors can increase the risk of developing leg ulcers:
- History of varicose veins or deep vein thrombosis
- Lack of physical exercise
- Arterial hypertension or diabetes
- Being overweight
- Smoking and alcohol abuse
How is a venous leg ulcer treated?
The sooner the ulcer is treated the faster it will heal.
Venous leg ulcers or predominantly venous leg ulcers must be treated by a doctor. Treatment generally begins with careful wound cleansing with soap and water or saline solution, without it needing disinfecting (using an antiseptic may imbalance the skin’s flora and slow down the healing process, or even cause an allergy). It is also essential to apply an appropriate dressing. Healthcare professionals should prescribe patients a dressing to reduce the healing time, based on the available clinical evidence.
The treatment should include the use of suitable compression bandages during the healing process, followed by lifelong use of compression socks. The good news is that with compression, venous leg ulcer relapse can be avoided by up to 90%; in contrast, without it, the relapse rate can reach 97%*.
In the event of a mixed leg ulcer (both venous and arterial), compression can be indicated but it will be looser than for a venous ulcer. It will depend on the degree of associated arteriopathy.
Compression is not indicated in arterial ulcers.
Avoiding relapse
Taking care of general health is the best way of preventing a leg ulcer from recurring:
- Taking regular walks to stimulate blood flow
- Wiggling, curling and pointing the toes while seated
- Rotating the ankle in both directions
- Avoiding sitting cross-legged
- Avoiding hot baths
- Wearing compression socks
- Wearing comfortable, non-slip shoes
- Regularly moisturising the skin
- Adopting a balanced diet and a healthy lifestyle (drink plenty of water, stop smoking)
- Preventing weight gain

